How fat-reducing treatments can be an option for chin augmentation
Learn how fat-reducing injections work as an alternative to chin liposuction for those considering options for chin augmentation procedures.
Dr Michael Rich is a specialist dermatologist who has been performing tumescent liposuction for over 30 years. Find out if Liposuction is suitable for you at ENRICH Clinic.
At ENRICH Clinic, we have a wide range of dermatological and cosmetic body treatments tailored to individual body and patient needs.
At ENRICH Clinic, our treatments are performed by our medical team consisting of doctors, nurses, and dermatologists and are tailored to each patient’s skin health needs.
ENRICH Clinic is committed to your skin health and well-being with a range of dermatological & cosmetic treatments tailored to the individual. Our treatments are performed by our medical team consisting of doctors, nurses, and dermatologists.
Skin health is essential for everyone. ENRICH Clinic has a wide range of technologies and dermatological solutions to help you achieve your skin care goals.
If you have a scar that’s thicker and raised compared to normal scars, you could have hypertrophic scars. While not dangerous, they can be a concern due to their appearance and, sometimes, discomfort.
The good news is hypertrophic scars can respond well to various treatment options, but it’s crucial to consult a healthcare professional for proper diagnosis and personalised guidance. Self-treating these scars can be counterproductive and even harmful. The following sections will explain why.
When you get a wound, your body goes through three healing stages:

The first stage, inflammation, is crucial for how your scar will turn out. Some chemicals called cytokines help control this process. In normal healing, the balance between “pro-inflammatory” cytokines (that cause inflammation) and “anti-inflammatory” cytokines (that calm things down) is important. If this balance is off, it can lead to thicker, raised scars like hypertrophic scars or keloids.
In the second stage, a protein called TGF-beta tells the fibroblasts how much collagen to make. In normal healing, TGF-beta levels are just right. But in hypertrophic scars and keloids, fibroblasts produce too much collagen.
This abnormal response to wound healing is more common after deeper wounds, like those from surgery, burns, or tattoos. People with specific genes, skin colours, or ages (younger adults) are more likely to get them. They also tend to show up more in certain regions of the body.
Both keloids and hypertrophic scars are raised, thickened formations that develop after skin injury or surgery. But, there are some key differences between the two:
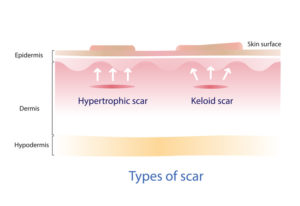
Here’s a table summarising the key differences:
| Feature | Keloid | Hypertrophic scar |
| Growth | Extends beyond wound | Confined to wound |
| Appearance | Red/pink/purple, smooth/shiny | Red/pink, bumpy/ridged |
| Progression | Continues growing | Reaches peak size, stabilises/flattens |
| Treatment | More challenging | Responds better |
| Skin types | More common in III-VI | May be more common in darker skin tones |
| Genetic link | Strong | None identified |
| Collagen arrangement | Haphazard | Parallel |
Note that these are general guidelines, and there can be some overlap in the characteristics of keloids and hypertrophic scars. These two can also be mistaken for something else, such as:
These “mimickers” pose a risk in treating keloids or hypertrophic scars because what helps one can be harmful to the other. For example, corticosteroids, which are often used to reduce keloid appearance, can worsen DFSP.
If you have a raised scar, it’s best to consult with a dermatologist or other healthcare professional for a proper diagnosis and treatment plan.
While hypertrophic scars themselves won’t completely disappear, they often improve significantly, even without treatment, becoming less noticeable and flatter. This process can take weeks to months, depending on the size and location of the scar.
If the scar is located on a joint or other area that restricts movement or you’re bothered by the scar’s appearance, various treatments can help.
Corticosteroids, given every few weeks for several months, are often the first-line treatment for hypertrophic scars. They reduce inflammation and collagen production, helping to flatten and soften the scar.
If your scar is stubborn, steroids may be given with fluorouracil to inhibit cell growth, preventing excessive scar tissue formation.
This noninvasive approach uses targeted laser beams to remove excess scar tissue and stimulate collagen remodelling. Different types of lasers–pulsed dye and fractional ablative– are used depending on the scar’s characteristics.
A newer option with promising results is radiofrequency ablation. This technique uses radio waves to heat and destroy scar tissue, potentially reducing its size and thickness.
This minimally invasive procedure involves creating tiny punctures in your scar tissue with fine needles. This stimulates collagen production and improves the scar’s texture and appearance.
Surgery might be considered in rare cases if other options haven’t been successful or if the scar significantly impacts movement. This can involve scar excision and reconstruction, followed by additional treatments to minimise scar formation.
The best treatment for your hypertrophic scar depends on its specific characteristics, individual goals, and doctor’s recommendations. At ENRICH, treatments range from laser and radiofrequency to micro-needling but can involve several effective treatment strategies.
Contact us to talk about your scarring, and we’ll put together a plan to help your skin health.
*With all surgeries or procedures, there are risks. Consult your physician (GP) before undertaking any surgical or cosmetic procedure. Please read the consent forms carefully and be informed about every aspect of your treatment. Surgeries such as liposuction have a mandatory seven-day cooling-off period to give patients adequate time to be sure of their surgery choice. Results may also vary from person to person due to many factors, including the individual’s genetics, diet and exercise. Before and after photos are only relevant to the patient in the photo and do not necessarily reflect the results other patients may experience. Ask questions. Our team of dermatologists, doctors and nurses are here to help you with any of your queries. This page is not advice and is intended to be informational only. We endeavour to keep all our information up to date; however, this site is intended as a guide and not a definitive information portal or in any way constitutes medical advice.
"*" indicates required fields
Combining Dr Rich’s dermatological skill with his knowledge of restorative skin regimes and treatments, the ENRICH range is formulated to help maintain and complement your skin. Our signature Vitamin C Day & Night creams are now joined by a Vit A, B,&C Serum and a B5 Hyaluronic Gel, both with hydration properties and much, much more.

Learn how fat-reducing injections work as an alternative to chin liposuction for those considering options for chin augmentation procedures.

Learn about surgical and non-surgical treatments available for platysmal bands, which are the vertical lines that appear on our necks as we age.

We talk about three non-surgical gummy smile treatments, including dermal fillers, anti wrinkle injections, and TADs.
Subscribe to the ENRICH newsletter and receive latest news & updates from our team.
Enrich Clinic acknowledges the Traditional Lands of the Wurundjeri Woi Wurrung and Bunurong peoples of the East Kulin Nations on which we work and trade. We pay respect to their Elders past, present and emerging. We extend our acknowledgement and respect to the LGBTQIA+ community who we welcome and support. Read our full Acknowledgement Statement here